Two-piece ceramic implant: Individual fully digital solution for highly aesthetic results in the anterior region
Case report by Dr. Claudia Michl, M.Sc.
This case report first appeared in the magazine ceramic implants 2024/1.
Introduction
Dental implants made of high-performance ceramics or zirconium oxide implants have now also become established for patients with special aesthetic requirements. Replacing an anterior tooth with implants places very high professional demands on the dentist. It is therefore particularly important to carry out precise planning prior to tooth extraction and implant placement in order to achieve predictably attractive results.
However, the use of ceramic implants not only offers aesthetic advantages, but also the possibility of offering patients a metal-free restoration. Especially in patients with proven titanium intolerance and an increased individual genetic tendency to inflammation, there is a 6-fold increased risk of primary or secondary loss of the titanium implant (4). In addition, the risk of peri-implantitis is significantly reduced due to the good biological compatibility of zirconia ceramics. Various studies have demonstrated a high survival rate of over 94% after 9 years (1), a low BOP and stable gingival conditions in the implant area even after many years.
Clinical situation and treatment planning
Anamnesis
The 38-year-old patient presented at my practice on 3 November 2020. His main problem was discomfort in tooth 11, which had undergone root canal treatment several years ago and had been causing discomfort for two years. These manifest themselves in a permanent latent bite pain on tooth 11 and sometimes pressure on the neighbouring tooth 21. In addition, tooth 11 sometimes seems to leak pus and blood.
Clinical examination

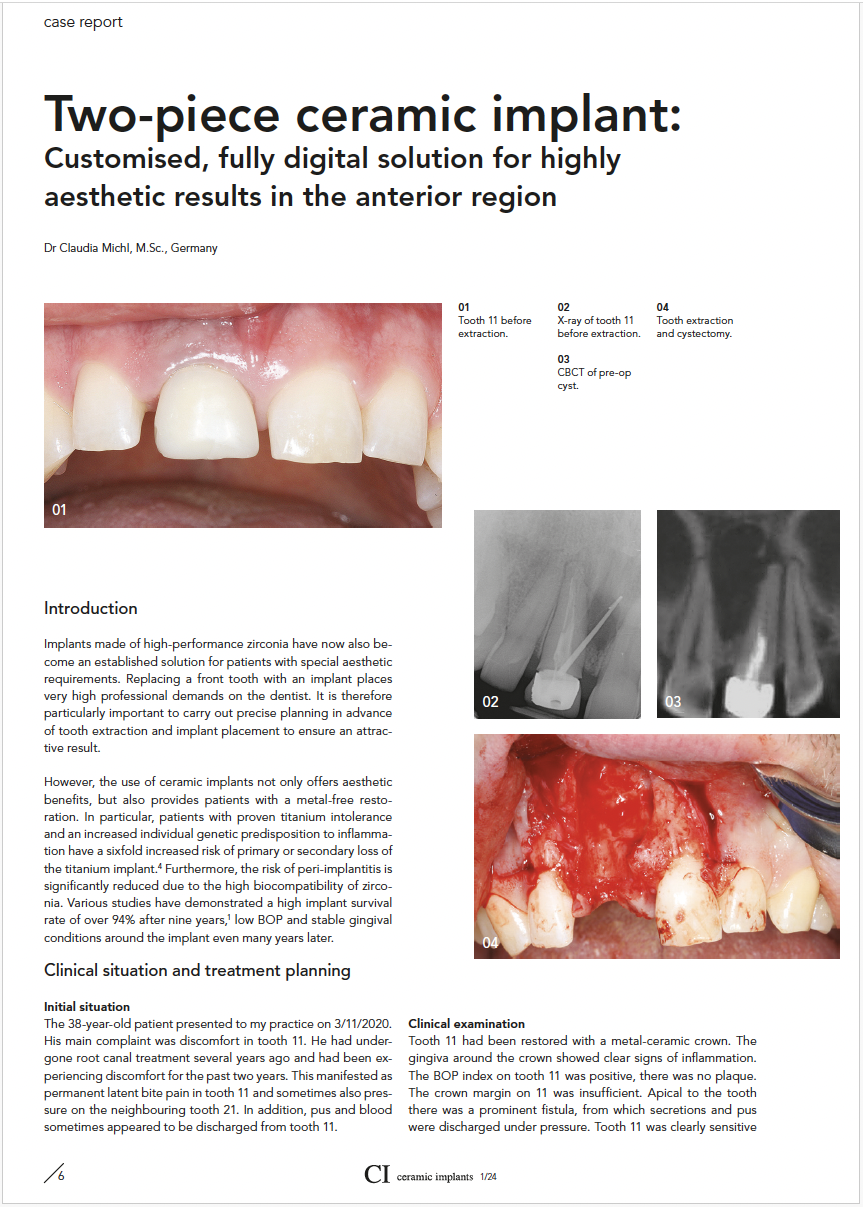
Figure 1: Tooth 11 before extraction
Tooth 11 is restored with a metal-ceramic crown. The gingiva around the crown shows clear signs of inflammation. The BOP index on tooth 11 is positive, there is no plaque. The crown margin on tooth 11 is insufficient. Apical to the tooth, a fistula is prominent, from which secretions and pus are discharged under pressure. Tooth 11 is clearly sensitive to percussion. The neighbouring teeth are insensitive to percussion tests and sensitive to cold stimuli. The periodontal screening index is 2 in all sixth teeth and the oral hygiene can be classified as good. The occlusion shows Class I interdigitation with a very patchy maxillary and mandibular front. The vertical relation is low. The overbite is 4 mm, the overjet 1.5 mm. The canines show clear signs of abrasion. The CMD screening test according to Ahlers and Jakstat showed no evidence of arthrogenic or myogenic dysfunction.
Radiological examination

Figure 2: X-ray of tooth 11 before extraction
The single-tooth image shows an endodontically treated tooth 11 with a gutta-percha point inserted into the fistula tract. Bone lightening can be seen around the gutta-percha point, which, starting apically from tooth 11, clearly takes up space interradicularly between 11 and 21. Based on these radiological findings, a CBCT with a FOV of 80 mm x 90 mm was performed.

Figure 3: CBCT pre-op cyst
The CBCT shows a very extensive interradicular hypodensity in region 11.21 starting from tooth 11. The dimensions of the interradicular area with low bone density measured from coronal to apical are 19.4 mm and from mesial to distal 10.9 mm. The buccal bone lamella is extremely thin and no more bone is detectable buccally in the area of root 11. A small hyperdense figure, which can be interpreted as displaced, overpressed root filling material, is prominent cranial to the whitening. Diagnosis: Insufficient crown 11 and radicular cyst originating from tooth 11 with buccal fistula.
Treatment procedure
Based on the findings and in consultation with the patient, the following treatment steps were taken:
1. Removal of tooth 11 with simultaneous cystectomy and reconstruction of the bone defect as well as fabrication of a temporary restoration (aesthetic splint, Erkodent)
2. Insertion of a two-part ceramic implant (Zeramex XT, CeramTec Switzerland) 4 months after augmentation
3. Restoration of the implant with a crown
As the patient has several allergies, a lymphocyte transformation test (LTT) and a basophil degranulation test (BDT) were carried out in order to rule out type I or VI allergies to the bone replacement material Bio-Oss (Geistlich) in advance. Blood samples were taken in our practice and analysed by the IMD laboratory in Berlin. No type I or VI allergy to Bio-Oss was detected.
The patient was premedicated 5 days preoperatively to 5 days postoperatively with Amoxiclav 500 mg 3 times a day, prednisolone 60 mg 1 h preoperatively as a single dose. For postoperative pain prophylaxis and anti-inflammatory therapy, a procaine base infusion (4 ml 2% procaine, 100 ml 8.4% sodium bicarbonate and 100 ml physiological saline solution) was administered during the operation and ibuprofen 600 mg for 4 days postoperatively as well as 20 mg pantoprazole once daily to support the gastric mucosa.
Tooth removal and cystectomy were performed as atraumatically as possible and without complications. This resulted in complete buccal fenestration, leaving a three-walled bone defect.

Figure 4: Tooth removal and cystectomy
This was reconstructed using the bone replacement material Bio-Oss, which was biologised with autologous bone in a ratio of 2:1 and PRF (platelet-rich fibrin). In addition, the augmentation material was treated with metronidazole powder for antimicrobial prophylaxis. After augmentation, an Ossix Plus membrane (Regedent) and Plasmamatrix PRF, which is rich in growth factors, were applied. To ensure tension-free, primary wound closure, the periosteum of the buccal flap was stretched using the ST-UP TM Soft Brushing Kit from Dr. Josef Choukroun.

Figure 5: Soccet Preservation Bio-Oss
The histological examination of the removed cyst tissue confirmed the suspected diagnosis of a radicular cyst. After wound healing without complications, the sutures were removed 14 days postoperatively.
No complications occurred during the further healing process and the CBCT taken 4 months after the operation shows a well-consolidated augmentation. Bone continuity was almost completely restored both buccally and crestally.
It was therefore possible to proceed with the insertion of a two-part ceramic implant made of hard zirconium dioxide ATZ ceramic (Zeramex XT 10 mm RB, CeramTec Switzerland).
Premedication was performed before implant placement according to the protocol of J. Choukroun. This was as follows: 1000 mg azitromycin the evening before the operation, 60 mg prednisolone 1 hour preoperatively and for pain medication and anti-inflammatory therapy until four days after the operation, 600 mg ibuprofen three times a day, and 20 mg pantoprazole once a day.
The implant bed preparation was performed according to the surgical drilling protocol. The pilot drilling was fully navigated using digitally planned and 3D-printed drilling templates. The surgical guide was planned after a previous intraoral scan (Trios III Fa 3Shape) and a DVT image (PaX-i3D Green, Vartech) by the Dentalmanufaktur Norbert Delly Bad Aibling laboratory using 3shape's implant studio. The implant bed was drilled to a depth of 11.5 mm to accommodate a 10 mm implant. The implant, biologised with PRF, was inserted at bone level with 30 Ncm. Primary wound closure was performed. The healing process was without complications.
After a healing phase of 4 months, there was a slight vertical bone loss of approx. 0.6 mm at the crest. This corresponds to the expected bone remodelling effect (2).

Figure 6: Implant in situ 4 months after bone augmentation
During uncovery, the implant was sealed with a 3 mm high gingiva former. This was customised with flowable composite before insertion in order to create the best possible emergence profile.

Figure 7: Closure with a 3 mm gingiva former
The implant impression was taken using a 3D scan (Trios III). For aesthetic reasons and to optimise the emergence profile, a restoration with a custom-made abutment was selected, which was screwed onto the implant with a Vicarbo screw (carbon fibre-reinforced screw made of PEEK).

Figure 8: Customised abutment
The abutment was made of TZP ceramic in the colour A3. The all-ceramic crown (made of zirconium dioxide ceramic), manufactured by the dental manufactory Norbert Delly in Bad Aibling, vestibularly veneered with silicon disilicate ceramic using the cut-back technique, was placed semi-permanently with Tempond.

Figure 9: Implant crown after insertion

Figure 10: X-ray image after insertion of the crown
Clinical results
The result after insertion of the ceramic crown: inflammation-free soft tissue conditions. During the 1-year follow-up, there was no inflammation or issues with the implant or the prosthetic restoration.

Figure 11: Tooth 11 after a 1-year follow-up
Discussion
The Zeramex XT implant system is designed for a wide range of indications in dental implantology. The two-part design offers the familiar advantages of titanium implantology, such as unloaded healing, primary wound closure, single-stage augmentation procedures and maximum flexibility in various surgical and prosthetic applications. The bolt-like screw connection with the Vicarbo screw (carbon fibre-reinforced screw made of PEEK) also ensures a stable, secure abutment-implant connection that optimally resists biomechanical forces. Low-risk soft tissue management, customised shaping of the emergence profile and simple re-entry and repair options are also possible.
Strict adherence to biological principles as part of the pre- and post-operative protocol as well as the patient's individual and current immunological status (allergies, presence of chronic systemic diseases) play an important role in the success of the treatment. Proactive testing using LTT tests, BDT tests or effector cell typing to detect possible material incompatibilities is an important factor in the course of cases to be resolved.
In this context, an optimal supply of micronutrients such as vitamin D3, C, B6 and B12, boron, manganese and melatonin as well as an ‘anti-inflammatory diet’, which also includes a special form of intermittent fasting, should also be mentioned. Also helpful are locally effective additives such as the use of platelet rich fibrin (PRF), which is rich in growth factors. Anti-inflammatory and immunomodulating measures such as the administration of special antibiotics and anti-inflammatory drugs according to a fixed schedule round off the holistic approach in dental implantology (1).
All these measures ensure that the oxidative stress in the tissue is kept at a low level and thus provide the best possible support for bone remodelling during wound healing.
References
1. Brunello, G., Rauch, N., Becker, K., Hakimi, A. R., Schwarz, F., & Becker, J. (2022). Two‐piece zirconia implants in the posterior mandible and maxilla: A cohort study with a follow‐up period of 9 years. Clinical Oral Implants Research, 33(12), 1233-1244.
2. Choukroun, E., Surmenian, J., Simonpieri, A., & Choukroun, J. (2021). Oxidative stress and osteoimmunology: The two missing pieces of the oral osseointegration puzzle. Diabetes, 16, 17.
3. Fischer, J., Rohr, P. D. N., & Jensch Fischer, P. D. Vielleicht darf's auch glatt sein. Internet: https://dzw.de/osseointegration-bei-zirkonoxid-implantaten. Zuletzt aufgerufen am 30.04.24.
4. Jacobi-Gresser, E., Huesker, K., & Schütt, S. (2013). Genetic and immunological markers predict titanium implant failure: a retrospective study. International journal of oral and maxillofacial surgery, 42(4), 537-543.
About author
Dr Claudia Michl, M.Sc. is an implantologist, biological dentist specialising in preventive dentistry as well as conservative, prosthetic and surgical rehabilitation and runs a office in Kolbermoor (Germany). She is certified in general implantology (DGZI e.V.) and environmental dentistry (DEGUZ e.V.). She also holds a Master's degree in dental functional analysis and functional therapy (University of Greifswald). She is also a member of the DGZI, DEGUZ and DGAST.
Do you have any questions about the publications or would you like to find out more about the Zeramex XT implant system?
We welcome publications on the Zeramex XT implant system. If you would like to document and publish your case, please let us know using the contact form.
Contact form


